
What is Missingness in Healthcare?
Missingness is a term that encapsulates a persistent and troubling pattern—when individuals repeatedly miss healthcare opportunities, which can lead to adverse health outcomes. It is not just about missing an appointment; it is about missing care and support, often due to factors beyond an individual’s control. Research in Scotland has shown that nearly one in five people miss more than two GP appointments over a 3 year period. These individuals often face significant health challenges, high treatment burden, complex social circumstances, and an increased risk of premature mortality.
But missingness is not just about individuals. It is about systems. It is about how healthcare structures sometimes fail to accommodate the needs of the most vulnerable. The same patterns of missingness seen in general practice persist into secondary care, with some patients leaving hospital before their treatment is complete. This issue requires urgent attention from policymakers, healthcare professionals, and the communities we work with.
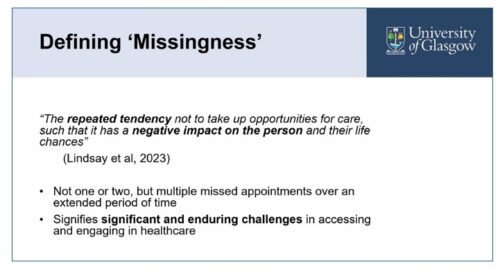
Defining missingness
Much of my work has been inspired by being involved in the General Practitioners at the Deep End group, who focus on providing care in the most socioeconomically deprived areas. Social determinants of health—such as poverty, unstable housing, and food insecurity—play a significant role in missingness. Addressing these determinants requires a shift in our healthcare approach. It is not enough to simply offer services; we must ensure that these services are accessible, welcoming, and designed to meet the needs of those who face the greatest barriers to care.
Barriers to Healthcare Access
There are numerous challenges that contribute to missingness. These include logistical barriers such as transportation, rigid scheduling, and a lack of flexibility in appointment systems. But the problem runs deeper—many people avoid healthcare due to past trauma, mistrust of the system, or the stigma they feel when seeking care.
“you see yourself as one of the least deserving people, when somebody reaches their haund…[…] because you believe already that you don’t deserve it, you arenae gonnae take the haund…”
Jim, Glasgow (quote from Missingness presentation)
VHS group discussion thoughts and ideas
I was struck by these key messages from VHS event group discussions around missingness which chimes with what we found in the research. The first is the importance of taking a trauma-informed, person-centred approach. This means understanding each individual’s unique circumstances and providing care that acknowledges past experiences and builds trust. It also means considering innovative ways to reach those at risk of missing care. For example, text message reminders can help, but we need to ensure they are delivered in a way that does not feel punitive or impersonal.
A Systems Approach to Addressing Missingness
Addressing missingness requires more than individual interventions—it demands a systemic shift. In the group discussion some solutions linked to the research were explored:
- Applying a “Missingness Lens”: Embedding an awareness of missingness in policy and practice can help us proactively identify at-risk individuals and develop interventions tailored to their needs.
- Community Link Workers (CLWs): These professionals play a crucial role in bridging the gap between healthcare services and the community. They help navigate systems, provide support, and connect individuals with appropriate resources. However, as highlighted in our discussion, their roles vary widely, and there is an urgent need to ensure their services are not diminished by funding cuts.
- Flexible Scheduling and Supportive Communication: Offering out-of-hours appointments, transport assistance, and a relational rather than transactional approach to healthcare can reduce multiple missed appointments.
- Inclusive Language and Training: Moving away from punitive terminology like “Did Not Attend (DNA)” to more person-centred language can help reduce stigma and foster engagement. Healthcare professionals also need training in inclusive and trauma-informed care.
 The Power of Lived Experience
The Power of Lived Experience
One of the most powerful aspects of the VHS group discussions also was the emphasis on lived experience. Listening to those who have experienced missingness firsthand is crucial in designing interventions that truly work. Healthcare systems should actively incorporate patient voices in policymaking and service design.
Moving Forward
Addressing missingness is not just about filling appointment slots—it is about reshaping healthcare to be more inclusive, accessible, and responsive to those who need it most. It is about creating a system that does not blame individuals for missing care but instead asks, “What can we do differently to support you?” If we want to address health inequalities, we must start by acknowledging and addressing missingness. The challenge is significant, but so is the opportunity to create meaningful change.
Professor Andrea Williamson is a GP and Professor of General Practice and Inclusion Health at the University of Glasgow.

This blog follows a presentation by Professor Williamson’s on Missingness at a Voluntary Health Scotland event- Read the Key Messages and view the event PowerPoint here.
